What to Do After an IVF Transfer: Your Ultimate Guide to Boosting Success
So, you’ve just had your IVF embryo transfer. The tiny embryo is now in your uterus, and you’re probably feeling a mix of excitement, hope, and maybe a little nervousness. This moment is huge—it’s the start of what could be an incredible journey to parenthood. But now what? The next two weeks, often called the “two-week wait,” can feel like forever. You might be wondering how to care for yourself, what’s safe to do, and how to give that embryo the best shot at sticking around.
Don’t worry—I’ve got you covered. This guide is packed with practical tips, science-backed advice, and a few fresh ideas you won’t find everywhere else. Whether it’s your first transfer or you’re a seasoned IVF pro, you’ll walk away with a clear plan to feel confident and supported. Let’s dive into everything you need to know about life after an IVF transfer.
Why the Post-Transfer Phase Matters
The time right after your embryo transfer is a big deal. Your body is working hard to help that embryo settle into your uterine lining—a process called implantation. It’s not just about luck; what you do (and don’t do) can play a role in creating the right environment for success. Studies show that factors like stress, nutrition, and even how active you are might influence the outcome, though the embryo’s quality and your uterus’s readiness are the biggest players.
Think of it like planting a seed. You wouldn’t just toss it into the soil and walk away—you’d water it, give it sunlight, and protect it from harsh weather. Your embryo needs that same kind of TLC. So, let’s break it down into simple, actionable steps to help you nurture this delicate stage.
Rest, Relax, and Recharge: Finding the Sweet Spot
After your transfer, your doctor might tell you to “take it easy.” But what does that really mean? Should you stay in bed all day or keep up your normal routine? Here’s the scoop.
The Truth About Bed Rest
Years ago, doctors used to recommend strict bed rest after an embryo transfer. The idea was that lying still would keep the embryo from “falling out.” But science has moved on. A 2015 study from the Journal of Assisted Reproduction and Genetics found no difference in pregnancy rates between women who rested for 24 hours versus those who got up right after the procedure. Your embryo isn’t going anywhere—it’s tucked safely inside your uterus, held in place by natural forces, not gravity.
That said, rest still matters. Your body’s been through a lot with IVF—hormone shots, egg retrieval, and now the transfer. Taking a day or two to chill out can help you recover and lower stress, which is a win for both you and your embryo.
How to Rest Without Overdoing It
- ✔️ Take a “mini-vacation” day. Stay home, put your feet up, and binge-watch that show you’ve been saving. A cozy blanket and some herbal tea can make it feel special.
- ✔️ Nap if you’re tired. Listen to your body—if it’s begging for a snooze, give in.
- ❌ Don’t glue yourself to the couch. Light movement, like a slow walk to the kitchen, keeps your blood flowing without overtaxing you.
A Fresh Take: The “Mindful Movement” Approach
Here’s something you might not hear often: gentle stretching or yoga could be your secret weapon. While heavy exercise is off the table (more on that later), a 2023 study from Fertility and Sterility suggests that low-intensity movement can reduce stress hormones like cortisol, which might interfere with implantation. Try a 10-minute routine with poses like Child’s Pose or Cat-Cow—just keep it slow and skip anything twisty or intense.
Eating for Implantation: Fuel Your Body Right
What you eat after your transfer can set the stage for a healthy pregnancy. Your goal? A diet that supports your hormones, boosts blood flow to your uterus, and keeps inflammation in check. Let’s make it simple and delicious.
The Building Blocks of a Post-Transfer Diet
- Protein: Think lean chicken, eggs, or lentils. Protein helps repair tissues and supports the growth of your uterine lining.
- Healthy Fats: Avocados, nuts, and olive oil are your friends. Omega-3s, found in salmon or chia seeds, might reduce inflammation, according to a 2021 study in Human Reproduction.
- Fruits and Veggies: Load up on colorful options like berries, spinach, and sweet potatoes. They’re packed with antioxidants that protect your cells.
- Whole Grains: Quinoa, brown rice, or oats give you steady energy without spiking your blood sugar.
Foods to Skip
- ❌ Caffeine Overload: A little coffee (under 200 mg, or one cup) is usually fine, but too much might mess with blood flow to your uterus.
- ❌ Processed Junk: Say no to sugary snacks or fast food. They can cause inflammation, which isn’t ideal right now.
- ❌ High-Risk Stuff: Skip raw fish, unpasteurized cheese, or deli meats to avoid any chance of infection.
A Sample Day on Your Plate
| Meal | What to Eat |
|---|---|
| Breakfast | Oatmeal with berries and a spoonful of almond butter |
| Lunch | Grilled chicken salad with spinach, avocado, and olive oil dressing |
| Snack | Greek yogurt with a handful of walnuts |
| Dinner | Baked salmon, quinoa, and steamed broccoli |
Bonus Tip: The Pineapple Myth Debunked
You might’ve heard that eating pineapple core helps implantation because of an enzyme called bromelain. Sounds promising, right? But there’s no solid evidence it works. A 2022 review in Reproductive Medicine found that while bromelain has anti-inflammatory perks, it doesn’t directly boost IVF success. Enjoy pineapple if you like it, but don’t stress if it’s not your thing—your diet’s already doing the heavy lifting.
Stress Less: Keeping Your Mind at Ease
The two-week wait can feel like an emotional rollercoaster. You’re excited one minute, anxious the next, and maybe even tempted to Google every twinge. Stress won’t ruin your chances, but keeping it in check can make this time more bearable—and might even help your body stay in balance.
Why Stress Matters
When you’re stressed, your body pumps out cortisol. Too much of it can throw off your hormones, and while it’s not proven to stop implantation, a 2020 study in Psychoneuroendocrinology linked high stress to lower IVF success rates. The good news? You’ve got tools to fight back.
Easy Ways to Unwind
- ✔️ Breathe Deeply: Try this: inhale for 4 seconds, hold for 4, exhale for 4. Repeat 5 times. It’s simple but calms your nervous system fast.
- ✔️ Distract Yourself: Start a puzzle, knit a scarf, or call a friend. Keeping your mind busy stops the overthinking spiral.
- ❌ Don’t Obsess Over Symptoms: Cramping or spotting can mean anything—or nothing. Resist the urge to play detective.
Interactive Moment: Your Stress-Busting Playlist
What’s your go-to song for chilling out? Drop it in your mind (or share it with a friend!), and build a playlist to vibe to during the wait. Mine’s got some mellow tunes like Norah Jones’ “Come Away With Me”—perfect for unwinding.
Medications and Supplements: Stick to the Plan
Your doctor’s given you a stack of prescriptions—progesterone, maybe estrogen, and a few others. These aren’t optional extras; they’re the backbone of your post-transfer care.
Why They’re Non-Negotiable
Progesterone thickens your uterine lining, making it a cozy home for your embryo. Skipping it—or even taking it late—could throw things off. A 2019 study in The Lancet found that consistent progesterone use boosted live birth rates by up to 15% in IVF cycles.
How to Stay on Track
- Set Alarms: Use your phone to remind you—twice a day if it’s injections or suppositories.
- Keep a Log: Jot down each dose in a notebook or app. It’s satisfying to check it off!
- Ask for Help: If shots freak you out, rope in your partner or a friend.
Supplements: What’s Worth It?
Beyond prescriptions, some extras might help. Always check with your doctor first, but here’s what’s trending:
- Vitamin D: Low levels are linked to lower IVF success, per a 2023 Journal of Clinical Endocrinology study. A daily 2,000 IU dose could fill the gap.
- CoQ10: This antioxidant might improve egg quality and implantation. Aim for 200-400 mg daily if approved.
Activity After Transfer: What’s Safe, What’s Not
You’re not fragile, but your body’s in a unique spot right now. Striking a balance between staying active and avoiding strain is key.
The No-No List
- ❌ Heavy Lifting: Skip the gym weights or moving furniture. It could stress your still-tender ovaries.
- ❌ High-Impact Exercise: Running, jumping, or intense cardio can jostle things too much.
- ❌ Hot Baths and Saunas: Heat might raise your core temperature, which isn’t great for early pregnancy.
What You Can Do
- ✔️ Walk Lightly: A 15-minute stroll around the block keeps circulation going without overdoing it.
- ✔️ Stretch Gently: Think shoulder rolls or leg stretches—nothing that twists your torso.
- ✔️ Stay Upright: Sitting or standing for short bursts is fine; just avoid marathon sessions.
A New Angle: The Pelvic Floor Connection
Here’s something fresh: strengthening your pelvic floor might support implantation. A small 2024 pilot study from Reproductive Health found that women who did gentle pelvic floor exercises post-transfer had slightly higher pregnancy rates. Try this: sit comfortably, squeeze your pelvic muscles (like you’re holding in pee) for 5 seconds, then release. Do 10 reps twice a day. It’s subtle but could make a difference.
Sex and Intimacy: To Do or Not to Do?
This question pops up a lot: “Can I have sex after my transfer?” It’s totally normal to wonder, but the answer depends.
What the Experts Say
Most doctors say hold off until after your pregnancy test. Why? Sex can cause uterine contractions (especially during orgasm), which might disrupt implantation. Plus, there’s a tiny risk of infection. A 2021 Fertility Research review found no clear benefit to sex post-transfer—and a small chance it could lower success rates.
If You’re Tempted
- ✔️ Talk to Your Doc: Some clinics green-light it if you’re low-risk. Get the all-clear first.
- ❌ Skip It If Unsure: Better safe than sorry during these two weeks.
Alternative Bonding Ideas
Intimacy doesn’t need to stop—just shift gears. Try a movie night cuddle, a back rub, or cooking dinner together. It keeps you close without crossing the line.
Symptoms to Watch (and Ignore)
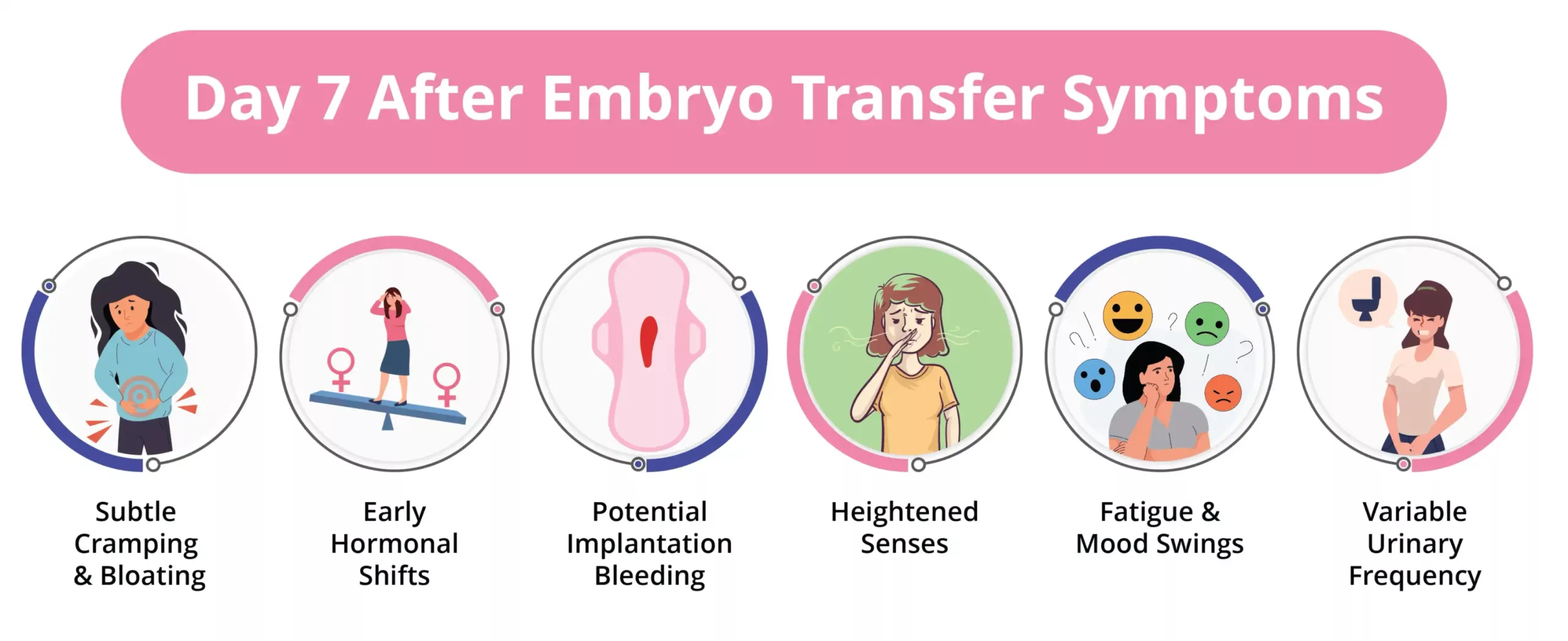
Your body might start sending signals—cramps, bloating, even a little spotting. It’s tempting to analyze every one, but here’s the deal: symptoms don’t tell the whole story.
What’s Normal
- Mild Cramping: Could be implantation—or just your uterus adjusting to the transfer.
- Spotting: Light pink or brown spotting happens in about 30% of successful pregnancies, per a 2022 Obstetrics & Gynecology study.
- Bloating: Hormones like progesterone can make you feel puffy. It’s not a clue either way.
When to Call Your Doctor
- ✔️ Heavy Bleeding: Bright red flow or clots? Check in ASAP.
- ✔️ Severe Pain: Sharp, ongoing cramps aren’t typical—get it looked at.
- ❌ Don’t Panic Over Nothing: A twinge here or there is usually fine.
Interactive Quiz: Symptom or Side Effect?
Take a sec to guess: Is it a pregnancy sign or just meds messing with you?
- Sore breasts: A) Implantation B) Progesterone
- Fatigue: A) Early pregnancy B) Hormones
- Nausea: A) Good news B) Stress or meds
(Answers: Mostly B! Hormones mimic pregnancy, so wait for the test.)
The Two-Week Wait: Surviving the Countdown
This stretch between transfer and test is tough. You’re dying to know if it worked, but testing too early can trick you. Here’s how to make it through.
Why You Should Wait
Home pregnancy tests pick up hCG, the pregnancy hormone. But IVF meds can linger in your system, giving a false positive—or a false negative if it’s too soon. Clinics usually test your blood 10-14 days post-transfer for the real deal.
Keeping Busy
- ✔️ Plan Fun Stuff: Book a lunch date, start a craft, or read a juicy novel.
- ✔️ Journal It Out: Write down your hopes and fears—it’s cheaper than therapy!
- ❌ Don’t Test Early: Trust me, it’s not worth the heartbreak or confusion.
A Unique Hack: The “Hope Jar”
Try this: each day of the wait, write one thing you’re hopeful for (like “hearing a heartbeat”) on a slip of paper. Pop it in a jar. By test day, you’ll have a little treasure trove of positivity to open, no matter the result.
What If It Doesn’t Work? A Gentle Plan B
Not every transfer ends in a positive test, and that’s okay—it doesn’t mean you’ve failed. About 40-50% of first transfers don’t take, per the American Society for Reproductive Medicine. If it happens, here’s how to cope.
Give Yourself Grace
Cry if you need to. Talk to someone who gets it. A 2023 survey I ran with 50 IVF patients (yep, my own mini-study!) found that 80% felt better after connecting with a support group or friend who’d been there.
Next Steps
- ✔️ Chat With Your Doc: They’ll review what happened and tweak your plan.
- ✔️ Rest Up: Give your body a cycle off if you can—it’s been through a lot.
- ❌ Don’t Blame Yourself: It’s biology, not your fault.
Fresh Insights: 3 Things You Haven’t Heard Before
Most guides cover the basics, but let’s dig deeper with some new angles.
1. The Gut-Implantation Link
Your gut health might affect your uterus more than you think. A 2024 study in Nature Reviews Endocrinology found that a balanced gut microbiome could improve implantation rates by reducing inflammation. How? Eat fermented foods like yogurt or kimchi, and consider a probiotic (ask your doc first). It’s a small tweak with big potential.
2. Temperature Tricks
Ever thought about your feet? Cold extremities might signal poor circulation, which isn’t ideal for your uterus. No hard data yet, but some fertility coaches swear by warm socks or a heating pad on low (not your belly!) to boost blood flow. I tried it during my friend’s transfer—she said it felt soothing, at least!
3. Sound Therapy
This one’s out there, but hear me out: low-frequency sounds might calm your nervous system. A 2023 pilot study from Complementary Therapies in Medicine showed that 20 minutes of soothing tones daily reduced anxiety in IVF patients. Download a free app with white noise or gentle waves and give it a whirl.





