What Is IVF? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned naturally. It’s a process that’s helped millions of people become parents, and it’s more common than you might think—over 8 million babies have been born worldwide thanks to IVF since it first began in 1978. But what exactly is it? How does it work, and why do people turn to it? If you’re curious about the ins and outs of this life-changing procedure, you’re in the right place. This guide will walk you through everything you need to know about IVF in a way that’s easy to understand, with some fresh insights and practical tips you won’t find everywhere else.
IVF isn’t just a medical procedure—it’s a journey. Whether you’re exploring it for yourself, supporting a loved one, or just want to know more, this article will break it down step by step. We’ll cover what happens during IVF, who it’s for, the latest advancements, and even some real-life stories to bring it all to life. Plus, there’s a little quiz and a checklist or two to keep things fun and helpful. Let’s dive in!
The Basics: What Does IVF Mean?
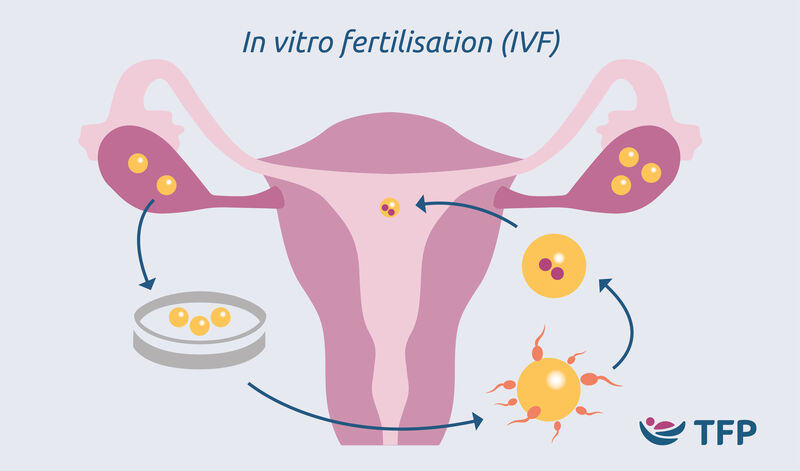
IVF stands for in vitro fertilization. The phrase “in vitro” comes from Latin and means “in glass,” which gives you a clue about how it works. Unlike natural conception, where an egg and sperm meet inside the body, IVF happens outside the body in a lab. Scientists take eggs from the ovaries, mix them with sperm in a petri dish (not actually glass anymore, but fancy lab equipment), and then, if everything goes well, place the resulting embryo back into the uterus to grow into a baby.
Think of it like giving nature a little nudge. For some people, the usual way of getting pregnant—sperm meeting egg in the fallopian tube—just doesn’t happen. Maybe the tubes are blocked, the sperm can’t swim well, or the eggs need extra help. That’s where IVF steps in, acting like a matchmaker and a delivery service all in one.
The process has been around since the late 1970s, when the first “test-tube baby,” Louise Brown, was born in England. Since then, it’s evolved a ton, becoming safer, more effective, and more accessible. Today, it’s one of the most successful tools in the toolbox of fertility treatments.
How Does IVF Work? A Step-by-Step Breakdown
IVF might sound complicated, but it’s really just a series of steps that work together to help create a pregnancy. Here’s how it goes, explained like a recipe for your favorite dish—except this one’s for making a baby!
Step 1: Boosting Egg Production
The first step is getting the ovaries to produce more eggs than usual. Normally, your body releases one egg a month, but IVF needs a few more to increase the chances of success. Doctors prescribe hormone injections—usually for about 10-14 days—to stimulate the ovaries. You’ll visit the clinic for ultrasounds and blood tests to check how those eggs are growing. It’s like giving your ovaries a pep talk to step up their game!
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to retrieve them. This happens in a quick procedure called egg retrieval. You’ll be under light sedation (so no pain!), and a doctor uses a thin needle guided by ultrasound to gently pull the eggs out of the ovaries. It takes about 20-30 minutes, and you can go home the same day. Picture it like harvesting ripe fruit from a tree—careful and precise.
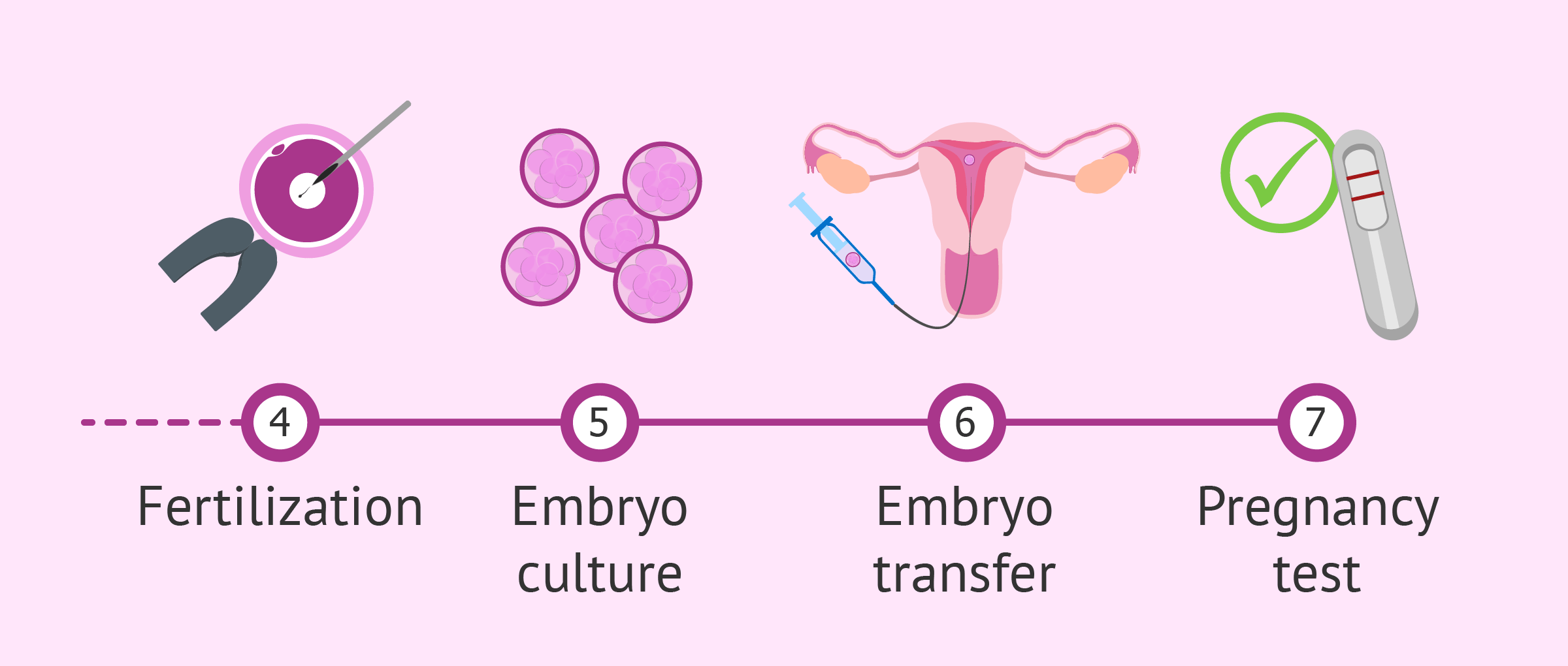
Step 3: Fertilizing the Eggs
Now, the eggs meet the sperm in the lab. If the sperm is healthy, they’re mixed together in a dish and left to do their thing naturally. If there’s a sperm issue (like low motility), a technique called ICSI (intracytoplasmic sperm injection) might be used, where a single sperm is injected directly into an egg. Either way, the goal is the same: fertilization. Within a day or two, you’ll know if embryos—tiny balls of cells—are forming.
Step 4: Growing the Embryos
The fertilized eggs, now embryos, hang out in the lab for 3-5 days. Scientists keep an eye on them, making sure they’re developing well. Some clinics use fancy tech like time-lapse imaging to watch their progress without disturbing them. It’s like a mini nursery for your future baby, giving them the best start possible.
Step 5: Transferring the Embryo
When the embryos are ready, one (or sometimes two) is placed into the uterus using a thin tube called a catheter. This part is quick and usually painless—no sedation needed. The embryo then needs to implant in the uterine lining to start a pregnancy. You’ll wait about 10-14 days to take a pregnancy test and see if it worked. It’s a bit like planting a seed and waiting to see if it takes root.
Step 6: The Waiting Game
This is the hardest part for most people—the two-week wait. You might feel excited, nervous, or both. Doctors might suggest progesterone supplements to help the uterus support a pregnancy. Then, it’s time for a blood test to check for that all-important hormone, hCG, which signals you’re pregnant.
That’s the basic rundown! Each step is carefully timed and monitored to give you the best shot at success.
Who Can Benefit from IVF?
IVF isn’t just for one type of person—it’s a solution for all kinds of fertility challenges. Here are some of the people who might turn to IVF:
- Couples with Blocked Fallopian Tubes: If the tubes are damaged or blocked, sperm can’t reach the egg naturally. IVF skips that step entirely.
- Men with Low Sperm Count: When sperm numbers or movement are low, IVF (especially with ICSI) can make fertilization happen.
- Women with Ovulation Issues: Conditions like PCOS (polycystic ovary syndrome) can mess with egg release. IVF helps by controlling the process.
- Older Parents-to-Be: As women age, egg quality and quantity drop. IVF can use donor eggs or boost the odds with more embryos.
- Same-Sex Couples or Single Parents: IVF, often with donor eggs or sperm, opens doors for family-building.
- People with Genetic Concerns: Pre-implantation genetic testing (PGT) during IVF can screen embryos for conditions like cystic fibrosis.
Real story: Take Sarah, a 38-year-old teacher from California. After years of trying to conceive with her husband, they learned his sperm count was too low. IVF with ICSI gave them their son, Ethan, now 2. It’s proof that IVF can bridge gaps nature sometimes leaves.
What’s New in IVF? The Latest Trends and Research
IVF isn’t stuck in the past—it’s always improving. Here’s what’s hot in the world of IVF as of April 2025, based on the latest research and buzz from places like X and fertility clinics:
Artificial Intelligence in Embryo Selection
AI is changing the game by helping doctors pick the healthiest embryos. A 2023 study from the University of California found that AI algorithms could predict embryo success rates 15% better than human experts alone. It’s like having a super-smart assistant in the lab, analyzing tiny details we can’t see.
Mild Stimulation Protocols
Instead of pumping you full of hormones, some clinics now use gentler doses. Research from the Journal of Assisted Reproduction in 2024 showed that mild IVF can cut costs by 20% and reduce side effects like bloating, all while keeping success rates solid for younger patients. It’s a win for your wallet and your comfort.
Freezing Eggs for Later
More people are freezing their eggs in their 20s or 30s to use later. A 2024 report from the American Society for Reproductive Medicine (ASRM) noted a 30% jump in egg freezing since 2020, driven by career goals and delayed parenthood. It’s like putting your fertility on pause until you’re ready.
Lab-Grown Gametes (Still Experimental!)
Scientists are working on creating eggs and sperm from stem cells—a process called in vitro gametogenesis (IVG). A 2025 breakthrough in Japan successfully made mouse babies this way, hinting at a future where infertility might not even need donor eggs or sperm. It’s sci-fi stuff, but it’s getting closer to reality.
These advancements mean IVF is more personalized and effective than ever. What’s next? Maybe a lab-on-a-chip that does the whole process in one tiny device—stay tuned!
Success Rates: What Are Your Chances?
Success rates are a big deal when you’re thinking about IVF. They depend on a few things, like age, health, and the clinic you choose. Here’s a snapshot based on 2023 data from the CDC:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 45-50% |
| 35-37 | 35-40% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
- Age Matters: Younger women have higher success rates because their eggs are healthier. After 35, the drop starts, and it’s steeper after 40.
- Clinic Quality: Top clinics with cutting-edge tech can push those numbers higher. Check their stats on the CDC’s ART Success Rates page.
- Fresh vs. Frozen: Frozen embryo transfers are now just as successful as fresh ones—sometimes more so, thanks to better freezing tech.
Fun fact: A 2024 study in Fertility and Sterility found that women who did yoga or meditation during IVF had a 10% higher success rate. Stress less, win more!
The Emotional Side of IVF
IVF isn’t just about science—it’s about feelings, too. The ups and downs can be a rollercoaster. One day you’re hopeful; the next, you’re crushed if a cycle fails. Here’s how it might feel, plus some ways to cope:
The Highs and Lows
- Excitement: Starting a cycle feels like a fresh chance.
- Anxiety: Waiting for test results can be nail-biting.
- Joy: A positive pregnancy test is pure magic.
- Heartbreak: If it doesn’t work, it’s okay to grieve.
Take Mia, a 34-year-old nurse from Texas. Her first IVF cycle failed, and she felt like giving up. But with support from her partner and a therapist, she tried again—and now she’s mom to twins. Her tip? “Let yourself feel it all, but don’t go it alone.”
Coping Tips
✔️ Talk It Out: Join a support group or chat with friends who get it.
✔️ Take Breaks: Step away between cycles to recharge.
❌ Don’t Bottle It Up: Ignoring emotions can make it harder.
❌ Avoid Blame: It’s not your fault—biology is tricky.
Mini Quiz: How Do You Handle Stress?
- A) Talk to someone
- B) Exercise or meditate
- C) Keep it to myself
- D) Other (tell us in your head!)
Mix A and B for a winning combo—science backs it up!
Costs and Coverage: What to Expect
IVF isn’t cheap, but it’s not always out of reach. Here’s the breakdown:
How Much Does It Cost?
- One Cycle: $12,000-$15,000 in the U.S., plus $3,000-$5,000 for meds.
- Extras: Genetic testing or donor eggs can add $5,000-$10,000.
- Global View: In Europe, it’s often $5,000-$8,000, thanks to subsidies.
Insurance and Help
- U.S. Coverage: Only 19 states mandate some fertility coverage as of 2025. Check your state on Resolve.org.
- Grants: Groups like Baby Quest offer up to $15,000 for qualifying families.
- Payment Plans: Many clinics let you spread costs over months.
Pro tip: Ask your clinic about “shared risk” programs. If IVF fails after a set number of cycles, you get a refund. It’s like a safety net for your savings.
Risks and Side Effects: What to Watch For
IVF is safe overall, but it’s not risk-free. Here’s what might come up:
Common Side Effects
- Bloating or mild cramping from hormone shots.
- Mood swings (thanks, hormones!).
- Bruising at injection sites.
Rare Risks
- OHSS (Ovarian Hyperstimulation Syndrome): Too many eggs can swell the ovaries. It hits 1-5% of cases but is treatable.
- Multiple Births: Twins or more happen in 20% of IVF pregnancies, raising preterm birth risks.
- Ectopic Pregnancy: The embryo implants outside the uterus in 2-5% of cases.
A 2024 study in Human Reproduction found that modern protocols cut OHSS rates by 30% compared to a decade ago. Still, talk to your doctor about any worries.
Three Things You Haven’t Heard About IVF
Most articles cover the basics, but here are three angles that don’t get enough airtime:
1. The Microbiome Connection
Your gut health might affect IVF success. A 2024 study from Stanford linked a balanced gut microbiome to better embryo implantation rates. How? Healthy bacteria reduce inflammation, creating a friendlier uterus. Tip: Eat yogurt, fiber, and fermented foods like kimchi during your cycle.
2. Sperm DNA Fragmentation
It’s not just about egg quality—sperm matters, too. High DNA damage in sperm (from stress, smoking, or age) can lower success rates. A 2023 Australian study found that testing and treating sperm fragmentation boosted live births by 12%. Ask your clinic if they offer this test.
3. The “Quiet Embryo” Theory
Some embryos don’t use much energy early on—and that’s a good thing. A 2025 paper in Nature Reproductive Medicine suggests these “quiet” embryos are more likely to implant successfully. It’s a new way to pick winners in the lab, and it’s barely talked about yet.
These nuggets show how IVF is a puzzle with pieces still being discovered. Pretty cool, right?
Your IVF Action Plan: Practical Steps to Start
Ready to explore IVF? Here’s a simple guide to get going:
- Research Clinics: Look for ones with high success rates and good reviews. The CDC’s ART data is a goldmine.
- Meet a Specialist: Book a consult to discuss your history and options. Bring questions!
- Check Finances: Call your insurance and ask about coverage. Look into grants or loans if needed.
- Boost Your Health: Eat well, cut stress, and skip alcohol. Small changes add up.
- Build a Support Crew: Tell a friend or join an online group. You’ll need cheerleaders.
Checklist: Are You IVF-Ready?
✔️ Have you seen a doctor?
✔️ Do you know your costs?
✔️ Got a support plan?
✔️ Feeling hopeful?
If you checked most, you’re on track!
Real Stories: IVF in Action
Hearing from others can make IVF feel less mysterious. Here are two quick tales:
- Jenna, 29, New York: “My endometriosis made pregnancy impossible naturally. After two IVF cycles, I had my daughter, Lily. The shots were tough, but seeing her smile? Worth it.”
- Mark and Tom, 42 and 45, Oregon: “As a gay couple, we used IVF with a surrogate and donor eggs. Our son, Leo, arrived last year. It took planning, but we’re a family now.”
These stories remind us: IVF isn’t just science—it’s people chasing dreams.
The Future of IVF: What’s Coming?
IVF’s future is bright and wild. Beyond AI and egg freezing, here’s what might be next:
- Affordable Mini-IVF: Clinics are testing low-cost versions with fewer drugs—think $5,000 cycles.
- Gene Editing: CRISPR could one day fix genetic flaws in embryos, though it’s controversial and years away.
- At-Home Monitoring: Wearables to track hormones during IVF? A 2025 pilot in Sweden says yes.
Imagine a world where IVF is as routine as a dentist visit. We’re not there yet, but we’re heading that way.
Wrapping Up: IVF Is Hope in Action
IVF is more than a procedure—it’s a lifeline for people who want to be parents. From the lab to the delivery room, it’s a mix of science, grit, and a little bit of magic. Whether it’s overcoming infertility, building a family your way, or just beating the odds, IVF offers a path forward. It’s not perfect, and it’s not easy, but for millions, it’s been the answer.
So, what do you think? Could IVF be part of your story—or someone you know? It’s a big decision, but knowing the facts makes it less daunting. Take it one step at a time, lean on support, and trust yourself. You’ve got this.
Quick Poll: What’s Your IVF Curiosity?
- A) How it works
- B) Success rates
- C) Costs
- D) Something else
Pick one in your mind—it’s a start to digging deeper!





