What Is In Vitro Fertilization (IVF)? A Deep Dive Into the Process, Science, and Real-Life Impact
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family, especially when things don’t go as planned naturally. It’s a process that’s helped millions of people become parents, but it’s also surrounded by questions, myths, and a bit of mystery. If you’re curious about what IVF really is, how it works, and what it means for those who choose it, you’re in the right place. This isn’t just a quick rundown—it’s a full-on exploration of IVF, from the science behind it to the emotional rollercoaster it can be, with some fresh insights you won’t find everywhere else.
IVF isn’t just a medical procedure; it’s a journey that blends cutting-edge technology with deeply personal hopes. Whether you’re thinking about it for yourself, supporting a loved one, or just want to understand this modern marvel, let’s break it down together—step by step, story by story, and fact by fact.
The Basics: What Does IVF Actually Mean?
IVF stands for in vitro fertilization, a fancy way of saying “fertilization in glass.” The “in vitro” part comes from Latin, meaning it happens outside the body, typically in a lab dish. Picture this: instead of an egg and sperm meeting inside a person’s body like they do in natural conception, scientists help them connect in a controlled environment. Once that happens, the fertilized egg—now an embryo—is placed back into the uterus to grow into a baby.
It sounds simple, right? But there’s a lot more to it. IVF is part of a bigger category called assisted reproductive technology (ART), which includes any method that uses medical tricks to help people conceive. Since the first IVF baby, Louise Brown, was born in 1978, over 8 million babies have come into the world this way. That’s a lot of little miracles!
So, who uses IVF? It’s for anyone facing challenges like blocked fallopian tubes, low sperm count, or unexplained infertility. It’s also an option for same-sex couples, single parents-to-be, or those wanting to avoid passing on genetic conditions. Basically, IVF steps in when nature needs a nudge.

How Does IVF Work? A Step-by-Step Journey
IVF isn’t a one-and-done deal—it’s a process with several stages, each one carefully timed and monitored. Here’s what happens, broken down into bite-sized pieces so you can follow along.
Step 1: Boosting Egg Production
The first step is all about getting the ovaries to produce more eggs than usual. Normally, your body releases one egg a month, but IVF needs a team effort. Doctors prescribe medications—usually injections you give yourself at home—to stimulate the ovaries. These meds, like follicle-stimulating hormone (FSH), tell your body, “Hey, let’s make a bunch of eggs this time!”
- What to Expect: You’ll visit the clinic for ultrasounds and blood tests to check how those eggs are growing. It’s like watching a garden bloom, but with high-tech tools.
- Fun Fact: A typical cycle might produce 10-15 eggs, though not all will be usable.
Step 2: Collecting the Eggs
Once the eggs are ready—usually after 8-14 days of stimulation—they’re collected in a minor procedure called egg retrieval. You’ll be under light sedation (no big surgery vibes here), and a doctor uses an ultrasound-guided needle to gently pull the eggs from your ovaries.
- Real Talk: It takes about 20-30 minutes, and you might feel crampy afterward, but most people are back to normal in a day or two.
- Pro Tip: Rest up and hydrate post-retrieval—it makes a difference!
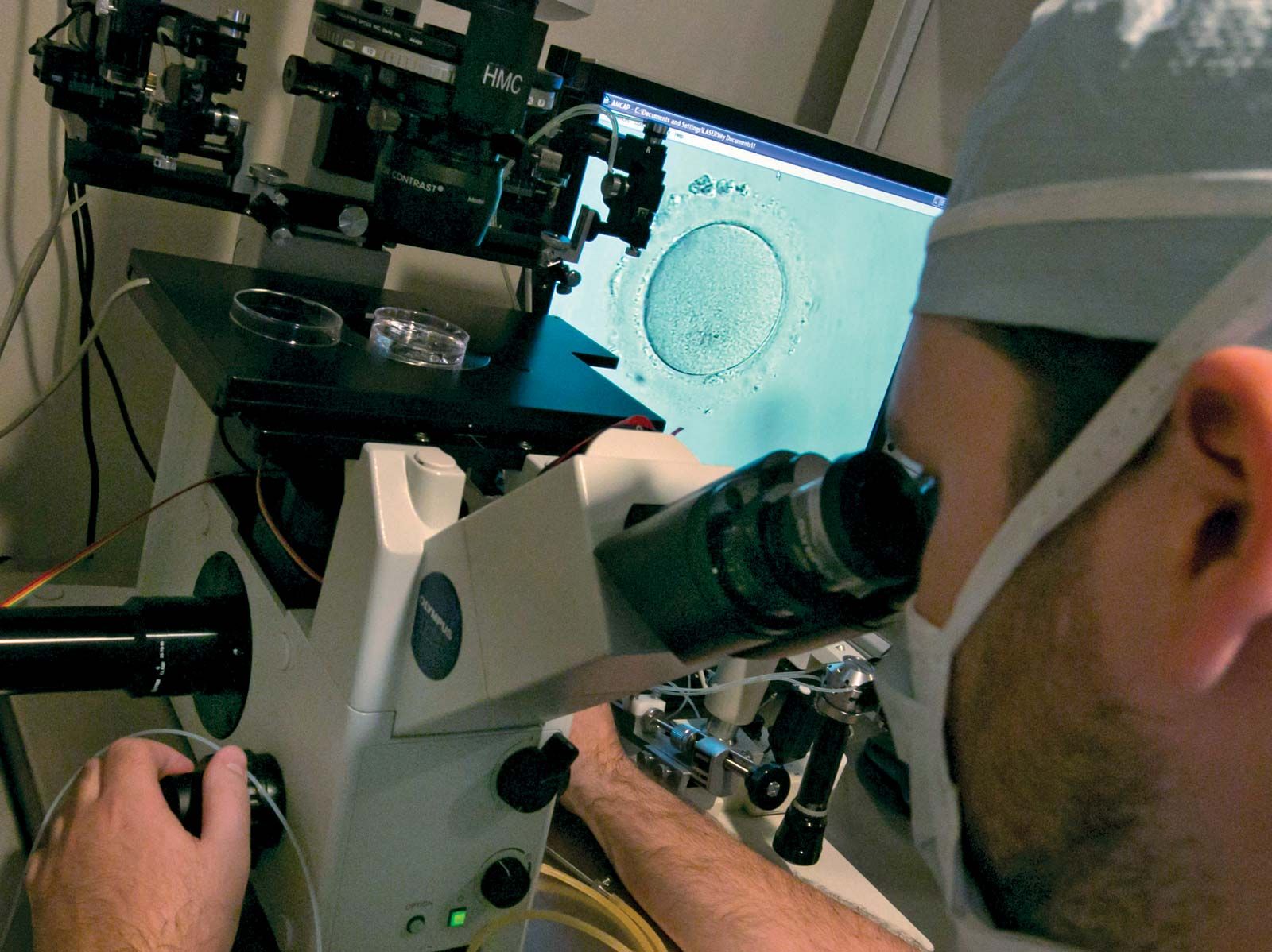
Step 3: Bringing Sperm and Egg Together
Now comes the magic moment. In the lab, the eggs meet the sperm. There are two ways this can happen:
- Traditional IVF: Sperm and eggs are mixed in a dish, and nature takes its course.
- ICSI (Intracytoplasmic Sperm Injection): If sperm need extra help, a single one is injected directly into an egg. This is common when sperm count or movement is low.
The goal? Fertilization. After a day or so, the lab team checks to see if it worked—did the egg and sperm become an embryo?
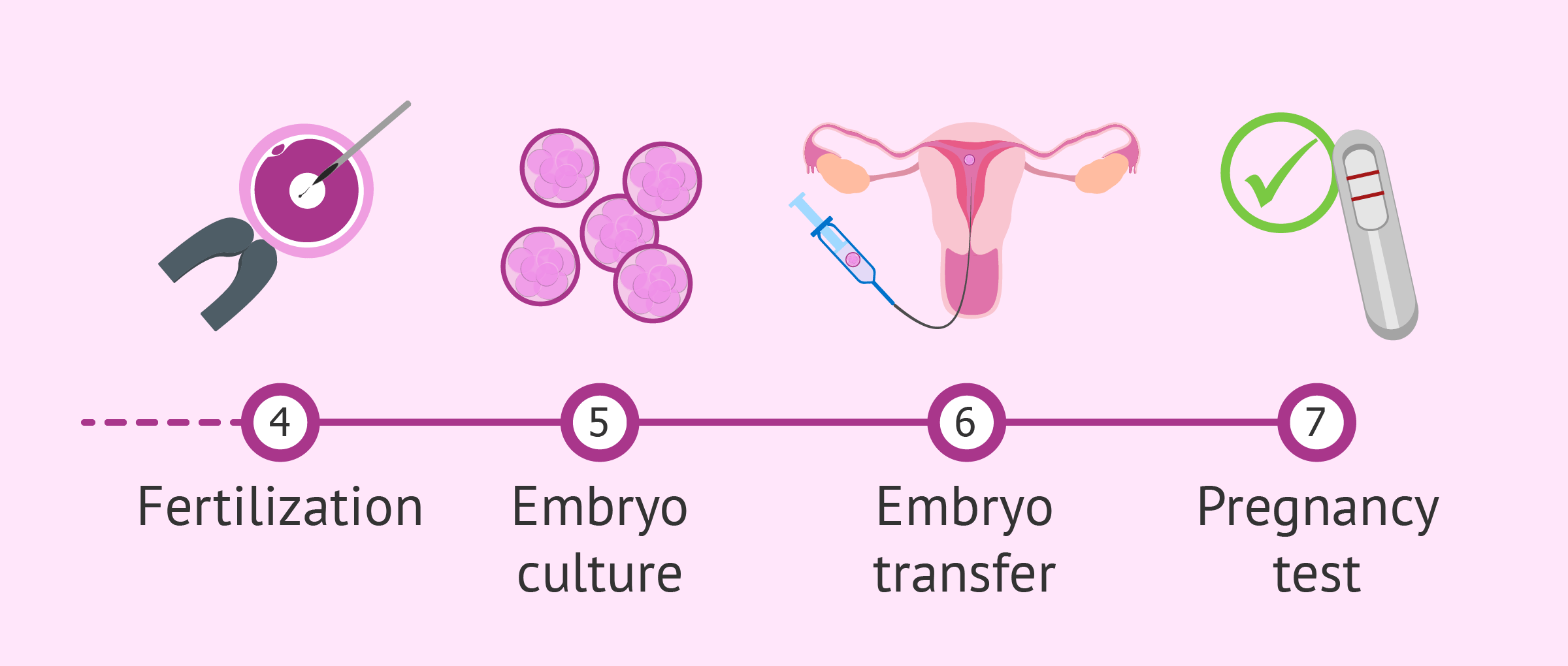
Step 4: Growing the Embryo
Fertilized eggs turn into embryos, and they’re nurtured in the lab for 3-5 days. Scientists watch them closely, making sure they’re dividing and growing strong. Some clinics use cool tech like time-lapse imaging to track progress without disturbing them.
- Did You Know?: By day 5, a healthy embryo might reach the blastocyst stage, which has a better shot at implanting in the uterus.
Step 5: Transferring the Embryo
Time to bring the embryo home! Using a thin tube called a catheter, the doctor places it into the uterus. It’s quick, painless, and done while you’re awake—no anesthesia needed. You might transfer one embryo or more, depending on your situation and doctor’s advice.
- Afterward: You’ll rest for a bit, then head home to wait—about 10-14 days—before a pregnancy test.
Step 6: The Waiting Game
This part’s tough: the two-week wait. You might feel hopeful, anxious, or both. A blood test will confirm if the embryo implanted and if you’re pregnant. If it works, congrats! If not, many try again—each cycle is a fresh chance.

What’s the Success Rate? Numbers That Matter
IVF success isn’t guaranteed, and it depends on a lot—like age, health, and even luck. Here’s a quick look at the stats, based on 2023 data from the CDC:
- Under 35: About 50% of cycles lead to a live birth.
- 35-37: Drops to around 38%.
- 38-40: Around 25%.
- Over 40: Closer to 10%, though using donor eggs can boost that way up.
What boosts your odds? Fresh embryos tend to do better than frozen ones (though freezing tech is improving fast), and younger eggs are key. Clinics also tweak protocols—like adjusting meds or timing—to fit each person.
Quick Quiz: What’s your guess—does IVF work better for younger or older folks? (Spoiler: Younger, but donor eggs can level the playing field!)
The Emotional Side: What IVF Feels Like
IVF isn’t just about needles and labs—it’s a wild ride emotionally. Imagine Sarah, a 32-year-old teacher who’s been trying to conceive for three years. She starts IVF full of hope, but the daily shots and constant checkups wear her down. When her first cycle fails, she’s crushed—but she tries again, because that’s what IVF often demands: resilience.
- The Highs: Seeing those eggs on an ultrasound, hearing “fertilization successful,” or getting that positive test.
- The Lows: Failed cycles, side effects like bloating or mood swings, and the cost piling up.
Tip: Build a support squad—friends, family, or even online groups. Talking it out helps. Studies show people who feel supported stick with IVF longer and handle setbacks better.
What’s New in IVF? Fresh Trends and Tech
IVF’s always evolving, and 2025 is no exception. Here’s what’s buzzing, based on recent chatter and research:
Microfluidics: The Future of Fertilization
Labs are testing tiny devices that mimic the body’s natural flow to sort sperm and grow embryos. It’s like a mini playground for cells, and early studies (like one from 2022 in Cureus) suggest it could make fertilization more efficient—fewer steps, better results.
Fertility Preservation Boom
More people are freezing eggs or embryos early, not just for medical reasons but as a “just in case” plan. Think of it like an insurance policy for your future family. Clinics report a 20% uptick in egg freezing since 2020, driven by folks delaying parenthood.
AI in the Lab
Artificial intelligence is popping up to pick the best embryos. It analyzes growth patterns faster than the human eye, and a 2023 study in Fertility and Sterility found AI-boosted cycles had a 15% higher success rate. Cool, right?
The Cost Factor: What You’re Really Paying For
IVF isn’t cheap—think $12,000-$25,000 per cycle in the U.S., not counting meds (another $3,000-$5,000). Insurance might cover some, but many pay out of pocket. Why so pricey? You’re funding high-tech labs, expert staff, and those custom meds.
- Money-Saving Hacks:
- Look for clinics with payment plans or discounts for multiple cycles.
- Check grants—groups like Baby Quest offer financial help.
- Consider mini-IVF (lower doses, lower cost) if it fits your case.
Poll Time: If you’ve done IVF, what surprised you most about the cost? Share in your head—or with a friend!
Risks and Realities: What to Watch For
IVF’s safe overall, but it’s not risk-free. Here’s what’s on the radar:
- Ovarian Hyperstimulation Syndrome (OHSS): Too much stimulation can swell your ovaries. It’s rare (1-5% of cases), but watch for bloating or pain—call your doc if it’s bad.
- Multiple Births: Transferring more than one embryo ups the chance of twins or triplets, which can mean preterm risks. Single embryo transfer (SET) is trending to avoid this.
- Emotional Toll: Stress and disappointment can hit hard. A 2021 study found 30% of IVF patients report anxiety spikes during treatment.
Practical Advice: Ask your doctor about SET if multiples worry you, and don’t skip self-care—yoga, walks, whatever keeps you grounded.
IVF Myths Busted: Separating Fact from Fiction
There’s a lot of noise about IVF. Let’s clear up some big ones:
- Myth: IVF babies are “unnatural.”
- Truth: They’re as natural as any baby—just conceived with a little help. No test-tube superpowers here!
- Myth: IVF always works on the first try.
- Truth: It’s more like a 50/50 shot under 35, and many need 2-3 cycles.
- Myth: It’s only for women with fertility issues.
- Truth: Men’s sperm problems are behind 40% of cases, and IVF helps all kinds of families.
Beyond Infertility: IVF’s Other Superpowers
IVF isn’t just for “fixing” infertility—it’s got broader uses that don’t get enough spotlight.
Dodging Genetic Diseases
Couples with conditions like cystic fibrosis can use preimplantation genetic testing (PGT) during IVF. It screens embryos for issues before transfer, cutting the risk of passing them on. A 2023 report showed PGT use jumped 25% in five years—huge for families with tough genetic histories.
Fertility After Cancer
Chemo can zap fertility, but freezing eggs or embryos beforehand gives survivors a shot at parenthood later. Take Mia, a 28-year-old who froze her eggs before breast cancer treatment. Two years later, she’s pregnant via IVF—a win science made possible.
Empowering Choice
Single folks and LGBTQ+ couples are turning to IVF with donor eggs, sperm, or surrogates. It’s not just about biology—it’s about building the family you want, your way.
A Day in the Life: What IVF Feels Like Up Close
Let’s walk through a cycle with Emily, a 35-year-old graphic designer. She’s on her second round after a failed first try.
- Week 1: Shots start. Emily’s nervous but sets reminders on her phone. Her partner helps with injections—teamwork!
- Week 2: Ultrasounds show 12 follicles growing. She’s bloated but excited.
- Retrieval Day: 10 eggs collected. She naps all afternoon.
- Day 5: Three embryos make it. One’s transferred, two are frozen.
- Two Weeks Later: Positive test! Emily cries happy tears.
It’s not all smooth—there’s fatigue, hope, and waiting—but for Emily, it’s worth it.
IVF Around the World: A Global Snapshot
IVF looks different depending on where you are. In the U.S., it’s mostly private and pricey. In places like Denmark, government funding covers three cycles—success rates there top 40%. Japan’s pushing “egg banking” for career-focused women, while India’s IVF boom (low-cost, high-quality) draws people globally.
Unique Insight: In 2024, Quebec’s public IVF program cut multiple births from 24% to 9% by prioritizing single transfers. Could the U.S. learn from that?
Your IVF Toolkit: Tips to Thrive
Ready to dive in? Here’s how to make it smoother:
✔️ Prep Your Body: Eat balanced meals, cut stress, and ask about supplements like CoQ10—some studies link it to better egg quality.
✔️ Ask Questions: What’s my clinic’s success rate? How many embryos will we transfer?
✔️ Lean on Tech: Apps like Flo or Ovia track your cycle and meds.
❌ Don’t Go Solo: Skipping support can make it harder—find your people.
❌ Avoid Overgoogling: Dr. Google’s not your doc—trust your team.
The Future of IVF: What’s Next?
IVF’s not standing still. Beyond AI and microfluidics, scientists are exploring in vitro gametogenesis—making eggs or sperm from skin cells. It’s years off, but imagine the possibilities for folks with no viable gametes. Plus, eco-friendly labs are cutting energy use, making IVF greener.
Mini Calculation: If costs drop 20% with automation (a real possibility by 2030), a $15,000 cycle could hit $12,000—still steep, but more doable.





