How IVF Works: Your Complete Guide to the Journey of In Vitro Fertilization
In vitro fertilization, or IVF, is like a helping hand for people dreaming of starting a family when nature needs a little nudge. It’s a process that’s been around for decades—since the first “test-tube baby,” Louise Brown, was born in 1978—and it’s helped millions of hopeful parents welcome babies into their lives. But how does it actually work? If you’re curious about the steps, the science, or what it feels like to go through it, you’re in the right place. This guide will walk you through everything, from the basics to the nitty-gritty details, with a few surprises along the way that you won’t find in every article out there.
IVF isn’t just a medical procedure; it’s a journey full of hope, patience, and sometimes a rollercoaster of emotions. Whether you’re exploring it for yourself, supporting a loved one, or just want to understand this incredible technology, we’ll break it down step by step. Plus, we’ll dive into some fresh insights—like how lifestyle tweaks can boost your chances, the latest tech making IVF smarter, and real stories from people who’ve been there. Ready? Let’s get started.
What Is IVF, Anyway?
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization outside the body.” In a nutshell, doctors take eggs from a woman’s ovaries, mix them with sperm in a lab, and then place the resulting embryo (a fertilized egg) back into the uterus to grow into a baby. It’s part of a bigger family of treatments called assisted reproductive technology (ART), designed to help when getting pregnant the usual way isn’t happening.
Think of it like baking a cake, but with a high-tech twist. Normally, the “ingredients” (egg and sperm) mix inside the body, and the “oven” (the uterus) does its magic naturally. With IVF, the mixing happens in a lab dish, and the oven gets a little prep work before the cake goes in. It’s a solution for all kinds of challenges—like blocked fallopian tubes, low sperm counts, or even unexplained infertility.
Over 10 million babies have been born through IVF worldwide, and it’s more common than you might think—about 2% of U.S. births today come from this process. It’s not a one-size-fits-all fix, but for many, it’s the key that unlocks the door to parenthood.

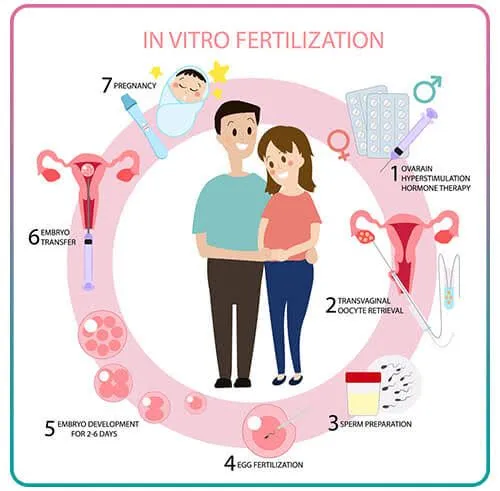
Step-by-Step: How IVF Brings a Baby to Life
IVF isn’t a quick fix—it’s a process that unfolds over weeks, sometimes months. Each step builds on the last, and while it’s guided by science, it’s also tailored to every person’s unique body. Here’s how it goes down, broken into bite-sized pieces so you can picture it clearly.
Step 1: Boosting Egg Production
The first part is all about getting those ovaries into gear. Normally, your body releases one egg a month during ovulation. With IVF, the goal is to produce several eggs at once to increase the odds of success. To do this, you’ll take hormone medications—usually shots you give yourself in the stomach or thigh—for about 10 to 14 days.
These hormones, like follicle-stimulating hormone (FSH), tell your ovaries, “Hey, let’s make more eggs!” Doctors keep a close eye on things with ultrasounds and blood tests to see how many eggs are growing and when they’re ready. It’s a bit like tending a garden—you water it, watch it sprout, and wait for the perfect moment to pick the flowers.
- What to Expect: Mild bloating or mood swings from the hormones are common, but most people manage just fine.
- Pro Tip: Keep a small cooler handy for your meds if you’re on the go—they often need to stay cold.
Step 2: Collecting the Eggs
Once the eggs are ripe (usually when they’re about 18-20 millimeters wide, tracked by ultrasound), it’s time for retrieval. This happens in a clinic, and you’ll be under light sedation—think of it like a nap where you don’t feel a thing. A doctor uses a thin needle, guided by ultrasound, to gently pull the eggs out of your ovaries through the vaginal wall. It takes about 20-30 minutes, and you’ll have 10-15 eggs on average, though it varies.
- Fun Fact: The eggs are tiny—about the size of a pinhead—but they’re packed with potential.
- Recovery Tip: Rest up afterward. A heating pad and some Netflix can make the day cozy while you recover from the sedation.
Step 3: Fertilizing the Eggs
Now the lab takes over. The eggs meet the sperm in a dish (not a test tube, despite the nickname!). There are two ways this can happen:
- Standard IVF: Sperm and eggs are mixed together, and nature takes its course as the strongest swimmers fertilize the eggs.
- ICSI (Intracytoplasmic Sperm Injection): If sperm need a boost (say, due to low count or poor movement), a scientist picks one healthy sperm and injects it directly into an egg with a tiny needle.
After a day or two, the team checks which eggs have fertilized and turned into embryos. It’s like waiting to see which seeds sprout in that garden we mentioned earlier.
Step 4: Growing the Embryos
The fertilized eggs—now embryos—spend 3 to 5 days growing in a special incubator. Scientists watch them closely, looking for signs of healthy development, like how many cells they’re dividing into. By day 5, the best embryos reach the “blastocyst” stage, which is prime time for transfer. If there are extras, they can be frozen for later use—more on that in a bit.
- Cool Tech Alert: Some clinics use time-lapse imaging to monitor embryos without disturbing them, giving a real-time peek at their progress.
Step 5: Transferring the Embryo
This is the big moment. A doctor uses a thin tube (catheter) to place one or two embryos into your uterus through your cervix. It’s quick—about 5-10 minutes—and you’re awake, no anesthesia needed. The embryo then needs to “stick” to the uterine lining, a process called implantation. You’ll rest for a bit after, but you can usually get back to normal the next day.
- What It Feels Like: Some say it’s like a Pap smear—mild cramping, but no big deal.
- Waiting Game: About 12-14 days later, a blood test confirms if you’re pregnant. This “two-week wait” can feel like forever, so plan some distractions!
Step 6: Supporting the Pregnancy
If the test is positive, you’ll keep taking progesterone (a hormone) for 8-10 weeks to help the embryo settle in. It’s like giving the uterus a cozy blanket to wrap around the new life. Regular checkups follow to make sure everything’s on track.
What Makes IVF Success Tick?
IVF isn’t a guaranteed win—it’s more like rolling the dice with better odds. Success rates depend on a bunch of factors, and here’s what the numbers say, based on 2021 data from the Society for Assisted Reproductive Technology:
- Under 35: About 45% of cycles lead to a live birth.
- 35-37: Drops to 32%.
- 38-40: Around 20%.
- 41-42: Down to 10%.
- Over 42: Just under 3%.
Age is the biggest player because younger eggs are usually healthier and more likely to implant. But it’s not just about age—here’s what else matters:
- Egg and Sperm Quality: Fresh, healthy ingredients make a better “cake.”
- Uterus Health: A welcoming environment helps the embryo stick.
- Lifestyle: Smoking, stress, and weight can nudge the odds up or down.
Quick Quiz: What’s Your IVF Vibe?
Take a sec to think about your situation. Answer these in your head:
- Are you under 35? (✔️ Better odds!)
- Do you eat well and stay active? (✔️ Bonus points!)
- Any past pregnancies? (✔️ Could mean a stronger chance.)
No pressure—just a fun way to connect the dots!
The Emotional Side of IVF
IVF isn’t just physical—it’s a mental marathon too. The ups and downs can hit hard, from the excitement of starting to the nail-biting wait for results. Plenty of people feel a mix of hope, anxiety, and even frustration if a cycle doesn’t work out.
Take Sarah, a 34-year-old teacher from Ohio. She went through three rounds of IVF before her son was born. “The first two failures crushed me,” she says. “But my husband and I leaned on each other, and finding a support group online kept me sane. It’s like you’re all in this weird club together.”
- Coping Tip: Try journaling or talking to someone who gets it. Online forums or local meetups can be goldmines for support.
- Reality Check: About 1 in 3 couples need more than one cycle, so patience is key.