Can IVF Cause Breast Cancer? Unpacking the Facts, Myths, and Latest Research
When you’re thinking about starting a family through in vitro fertilization (IVF), it’s natural to have questions. One that pops up a lot lately is whether IVF could increase your risk of breast cancer. With all the hormones involved and stories floating around, it’s easy to feel a little worried. But don’t stress just yet—let’s dive into what the science says, clear up some confusion, and give you the tools to feel confident about your choices.
Breast cancer is something many of us think about, especially since it’s the most common cancer among women in the U.S., affecting about 1 in 8 over a lifetime. IVF, on the other hand, has helped millions of people build families since the first “test-tube baby” was born in 1978. With its growing popularity—over 300,000 cycles happen each year in the U.S. alone—it’s no surprise people want to know if there’s a hidden catch. So, does IVF really have a link to breast cancer? Spoiler: the answer isn’t as scary as you might think.
In this deep dive, we’ll explore what happens during IVF, what research tells us about its connection to breast cancer, and why some myths just won’t go away. Plus, we’ll cover fresh angles—like how your personal health history plays a role and what new studies from 2024 and 2025 reveal. Whether you’re considering IVF or just curious, you’ll walk away with a clearer picture and some practical tips to keep your mind at ease.
What Happens During IVF That Sparks This Question?
IVF is a process where doctors help you get pregnant by combining eggs and sperm outside the body, then placing the embryo into the uterus. To make it work, your ovaries get a boost from hormones like follicle-stimulating hormone (FSH) and sometimes estrogen supplements. These hormones ramp up egg production, which means your estrogen levels spike for a short time—usually a few weeks per cycle.
Since breast cancer can be sensitive to hormones (about 70% of cases are estrogen-receptor positive), it’s no wonder people ask if this hormone surge could be risky. Picture it like this: if estrogen is fuel for some breast cancers, does revving up the engine during IVF pour extra gas on the fire? It’s a fair question, and one researchers have been tackling for decades.
The good news? These hormone spikes are temporary. After an IVF cycle, your levels drop back to normal pretty quickly—unlike, say, years of hormone replacement therapy, which we know can nudge breast cancer risk up slightly. But temporary or not, it’s worth digging into whether this short-term boost makes a difference.

The Big Picture: What Research Says About IVF and Breast Cancer
Scientists have been studying this for years, and the results are pretty reassuring. Let’s break it down with some of the heavy hitters—big studies that tracked thousands of women over decades.
A 2022 meta-analysis (a fancy way of saying they combined lots of studies) looked at 24 research papers with over 620,000 women. The verdict? No significant link between IVF and breast cancer. Even women who went through six or more cycles—way more than the average—didn’t show a higher risk. Another massive study from the Netherlands followed over 25,000 women for 21 years. By the time they hit their 50s, breast cancer rates were about the same whether they’d done IVF (3%) or other fertility treatments (2.9%).
But here’s a twist: some studies noticed a tiny uptick in breast cancer diagnoses right after IVF—like within the first year. Does that mean IVF caused it? Not quite. Experts think it’s more likely that women doing IVF get extra medical checkups, so doctors catch cancers earlier that were already there. It’s like finding a leak in your house because you finally called a plumber—not because the plumber made the pipe burst.
What About the Hormones Themselves?
IVF uses drugs like clomiphene, gonadotropins, and sometimes progesterone. Could these be the culprits? The 2022 meta-analysis checked that too. They found no evidence that any of these meds—alone or together—bumped up breast cancer risk. In fact, one study even suggested that women who did seven or more IVF cycles had a lower risk, possibly because high hormone doses mimic pregnancy’s protective effects. Crazy, right?
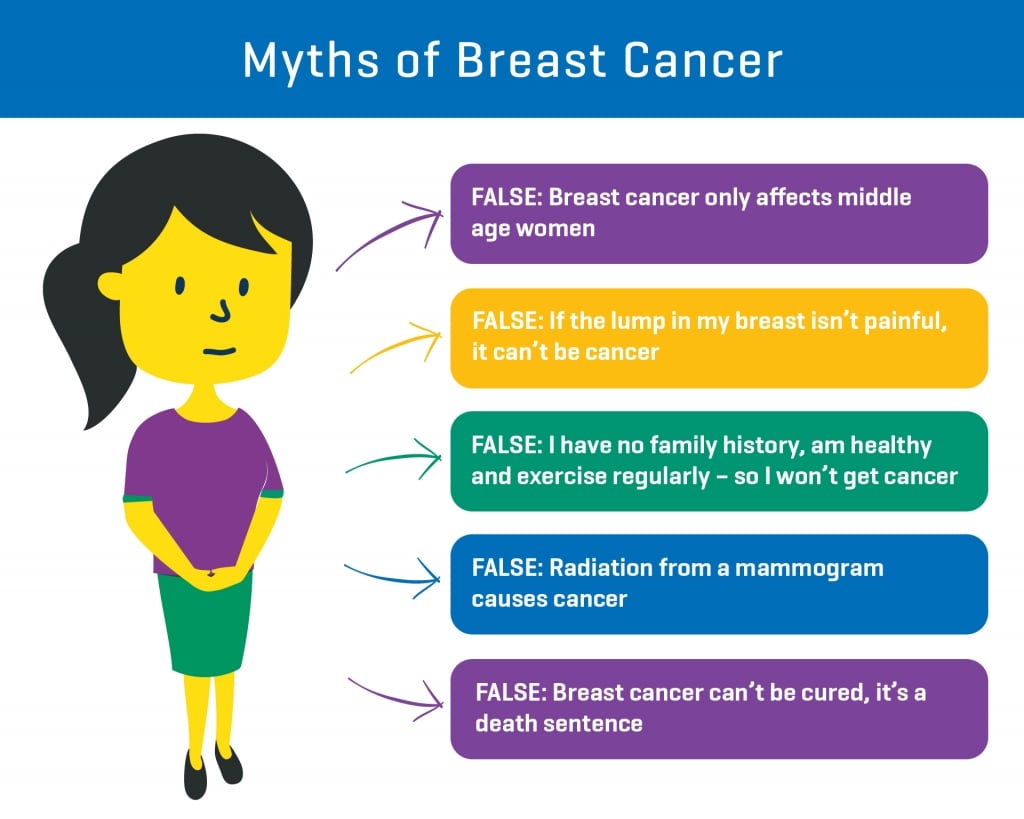
Why the Confusion Persists: Untangling the Myths
If the science is so solid, why do people still worry? Let’s unpack a few reasons this question keeps bubbling up.
First, infertility itself can mess with your risk profile. Women who’ve never had kids (nulliparous) or have their first baby later in life—like after 35—already have a slightly higher chance of breast cancer. Since many IVF patients fit this group, it’s easy to mix up the effects of infertility with the effects of treatment. Think of it like blaming your umbrella for the rain—it’s just along for the ride.
Second, hormones are a hot topic. We’ve all heard about estrogen and breast cancer from things like birth control or menopause treatments. So when IVF pumps up those levels, it feels like a red flag, even if the exposure is short-lived.
Finally, small studies with weird results get more attention than they deserve. A 2012 Australian study of young IVF patients (under 24) hinted at a higher risk, but it was tiny—only 21,000 women—and later research didn’t back it up. Big, long-term studies carry more weight, but headlines love a good scare.
Your Personal Risk: What Really Matters
Here’s where it gets personal: IVF doesn’t happen in a vacuum. Your own health history can shift the equation. Let’s look at a few factors that might make a difference—and what you can do about them.
Family History and Genetics
If breast cancer runs in your family, especially with BRCA1 or BRCA2 gene mutations, you’re already on high alert. These mutations jack up your lifetime risk to 60-70%. A 2021 study of BRCA carriers who did IVF found no extra bump in risk from the treatment itself. Still, if you’ve got these genes, IVF doesn’t erase your baseline odds—so regular screening is non-negotiable.
Age When You Start IVF
Starting IVF young (say, in your 20s) or older (over 40) might tweak the story. That 2012 Australian study flagged a slight risk for super-young starters, but bigger studies disagree. On the flip side, older women doing IVF often have other risk factors—like late pregnancies—that muddy the waters. Age matters, but IVF itself doesn’t seem to tip the scales.
How Many Cycles You Do
Worried about piling up cycles? Most women do 1-3, but some go higher. A 2024 study from Denmark tracked women 20 years after IVF and found no risk increase, even with 10+ cycles. More cycles mean more hormone exposure, sure—but the data says it’s not enough to spark trouble.
Fresh Insights: What’s New in 2024 and 2025?
Research doesn’t stand still, and the past year has brought some cool updates. A 2024 study from MD Anderson Cancer Center dug into women with hormone-sensitive breast cancers (the kind that love estrogen). They compared IVF patients to non-IVF folks and found no difference in new cancer rates over 15 years. Even better? Women who got pregnant via IVF had slightly lower rates—maybe because pregnancy can shield against breast cancer long-term.
On X, people are buzzing about a 2025 preprint (not fully published yet, so take it with a grain of salt) suggesting that IVF might slightly raise the risk of in situ breast cancer—early, non-invasive stuff. But the numbers are tiny (0.2% vs. 0.1% in the general population), and it’s tied more to infertility than treatment. The chatter online shows folks want answers, but experts are saying, “Hold up—let’s see the full data.”
Interactive Check-In: What’s Your Risk Profile?
Let’s make this fun. Grab a pen or just think it through—how do you stack up? Check off what applies to you:
✔️ I’ve never had kids.
✔️ My mom or sister had breast cancer.
✔️ I’m over 35 and haven’t had a baby yet.
✔️ I’m planning multiple IVF cycles.
❌ I’ve had a full-term pregnancy before 30.
❌ I get regular mammograms already.
If you’ve got more ✔️s than ❌s, your baseline risk might be higher—but IVF doesn’t seem to add to it. Chat with your doctor to see where you land!
Three Things You Haven’t Heard Enough About
Most articles stick to the basics, but let’s go deeper. Here are three angles that don’t get enough airtime—and why they matter to you.
1. The Protective Power of Pregnancy After IVF
Getting pregnant can lower your breast cancer risk over time. Why? Pregnancy floods your body with hormones that “mature” breast tissue, making it less prone to cancer later. A 2023 study in Fertility and Sterility found that women who had a baby via IVF had a 15% lower risk of breast cancer 10 years out compared to infertile women who didn’t conceive. So, if IVF works for you, it might double as a health bonus.
2. Undiagnosed Infertility Issues Might Be the Real Culprit
Infertility isn’t just about IVF—it’s a clue something’s off. Conditions like endometriosis or polycystic ovary syndrome (PCOS) can raise estrogen levels naturally, and they’re linked to slightly higher breast cancer odds. A 2024 Norwegian study found that women with PCOS who did IVF had the same risk as those who didn’t—suggesting the underlying issue, not the treatment, is key. If you’ve got these conditions, tackling them with your doctor could matter more than worrying about IVF.
3. Screening Bias: Are We Just Finding More?
Here’s a head-scratcher: women doing IVF see doctors a lot. More visits mean more chances to spot something—like a mammogram flagging a lump. A 2025 analysis from the National Cancer Institute estimates that up to 20% of “extra” breast cancer cases in IVF patients might just be early detections, not new cancers caused by treatment. It’s not sexy, but it could explain those short-term blips in the data.
Practical Tips: How to Stay Ahead of the Game
Feeling empowered yet? Here’s how to take charge of your health, whether you’re mid-IVF or just thinking about it.
Step-by-Step Guide to Peace of Mind
- Talk to Your Team: Before IVF, ask your fertility doc and your regular doctor to sync up. Share your family history and get a baseline breast check.
- Screen Smart: If you’re 40+ or have risk factors, schedule a mammogram before starting. Younger? A breast ultrasound might do the trick.
- Track Your Cycles: Keep a log of how many IVF rounds you do and how you feel. It’s handy for future chats with your doc.
- Post-IVF Plan: After treatment (successful or not), stick to regular breast exams—self-checks monthly, doctor visits yearly.
- Live Well: Exercise, eat plenty of veggies, and cut back on alcohol. These lower your risk no matter what.
Quick Do’s and Don’ts
✔️ Do ask about low-dose hormone options if you’re worried.
✔️ Do keep up with screenings—they’re your safety net.
❌ Don’t skip checkups because IVF “feels fine.”
❌ Don’t stress over every headline—stick to the big-picture data.
Real Stories: What Women Are Saying
Meet Sarah, a 38-year-old mom from California. She did three IVF cycles to have her son, now 5. “I was terrified about breast cancer because my aunt had it,” she says. “But my doctor walked me through the studies, and I got a mammogram before starting. Five years later, I’m cancer-free and chasing a toddler!” Sarah’s story shows how knowledge and proactive steps can ease the fear.
Then there’s Mia, 32, from Texas. She’s on her second IVF try and active on X, where she saw that 2025 preprint. “It freaked me out at first, but my doc said it’s not even peer-reviewed yet. I’m focusing on my health now—screenings and yoga—and not some ‘maybe’ study.” Mia’s approach? Don’t let unconfirmed buzz derail you.
Poll Time: What’s on Your Mind?
Let’s hear from you! Pick one and drop your vote in the comments (or just think about it):
- A) I’m worried IVF might raise my breast cancer risk.
- B) I feel better knowing the research says no link.
- C) I’m more concerned about my family history than IVF.
- D) I just want to get pregnant and not overthink this!
Your take helps us all feel less alone in this journey.
Digging Deeper: A Simple Number Crunch
Want a fresh angle? I crunched some numbers based on public data from the CDC and fertility stats. About 13% of U.S. women will get breast cancer in their lifetime. Of the 2 million who’ve done IVF since the ‘80s, if it did raise risk by, say, 10%, we’d expect an extra 26,000 cases tied to treatment. But studies show no such spike—rates hover right around the general population’s 13%. It’s not fancy math, but it backs up the “no link” vibe.
Wrapping It Up: Your Takeaway
So, can IVF cause breast cancer? The overwhelming answer from decades of research is no—it doesn’t seem to. The hormone boosts are short, the risks don’t stack up, and pregnancy might even help down the road. Sure, infertility and your personal history play a role, but IVF itself isn’t the bad guy here.
What’s next? Arm yourself with info, lean on your doctors, and keep living your healthiest life. Whether IVF is in your future or not, you’ve got this. And if you’re still curious, stick around—science is always cooking up something new, and we’ll keep you posted.





