How Does IVF Work? A Step-by-Step Guide to Your Fertility Journey
In vitro fertilization, or IVF, is like a lifeline for so many people dreaming of starting a family. It’s a process that blends science, hope, and a little bit of patience to help those who can’t conceive naturally. If you’ve ever wondered what happens behind the scenes—how eggs and sperm meet outside the body, how embryos grow, and how they make their way back to the womb—this guide is for you. We’re diving deep into every step, breaking it down so it feels less like a mystery and more like a journey you can picture yourself on. Plus, we’ll sprinkle in some fresh insights, practical tips, and the latest trends to give you a fuller, richer understanding of IVF in 2025.
What Is IVF, Anyway?
IVF is a fertility treatment where doctors help eggs and sperm come together in a lab, rather than inside the body. The term “in vitro” literally means “in glass,” which is a nod to the petri dishes used in the process. Once the eggs are fertilized and grow into embryos, one or two are placed into the uterus, hoping they’ll implant and lead to a pregnancy. It’s a solution for all kinds of fertility challenges—blocked fallopian tubes, low sperm count, or even unexplained infertility.
Think of it like a carefully choreographed dance: every step has to happen at just the right time, guided by medical experts and cutting-edge tech. It’s not a one-size-fits-all fix, but for many, it’s the key that unlocks the door to parenthood.
Why People Turn to IVF
Infertility affects about one in seven couples, and that number’s been climbing as more folks delay having kids for career or personal reasons. IVF steps in when nature needs a nudge. Maybe the ovaries aren’t releasing eggs, or the sperm can’t make the journey to meet them. Sometimes, it’s a mix of factors no one can quite pin down. Whatever the reason, IVF offers a workaround—a chance to build a family when the usual path isn’t working.
In 2025, we’re seeing more openness about fertility struggles, too. Social media buzz on platforms like X shows people sharing their IVF stories, swapping tips, and cheering each other on. It’s not just a medical process anymore—it’s a community.
Step 1: Getting Your Body Ready with Ovarian Stimulation
The IVF journey kicks off with ovarian stimulation. Normally, your body releases one egg a month, but IVF needs more to boost the odds of success. Doctors prescribe hormone injections—usually follicle-stimulating hormone (FSH) and luteinizing hormone (LH)—to coax your ovaries into producing multiple eggs.
How It Works
For about 8 to 14 days, you’ll give yourself these shots (don’t worry, the needles are tiny!). Your doctor keeps a close eye on things with blood tests and ultrasounds, tracking how your follicles (the sacs where eggs grow) are developing. When they’re big enough—around 18-20 millimeters—the eggs inside are ready to roll.
What It Feels Like
Some folks breeze through this, while others feel bloated or moody from the hormones. It’s like PMS on steroids for a couple of weeks. Hydration and rest can help, but it’s okay to lean on your support crew if you’re feeling off.
Fresh Insight: Mild Stimulation Trend
Here’s something new: in 2025, more clinics are offering “mild stimulation IVF.” It uses lower doses of drugs to get fewer eggs but with less strain on your body. Research from the American Society for Reproductive Medicine suggests it’s just as effective for some patients, cutting costs and side effects. Could it be right for you? It’s worth a chat with your doctor.
Step 2: Egg Retrieval—Harvesting the Goods
Once your eggs are ripe, it’s time for retrieval. This is a quick procedure, usually done under light sedation, so you’re snoozing through the whole thing.
The Process
A doctor uses an ultrasound-guided needle to gently pull the eggs from your ovaries. It takes about 20-30 minutes, and you’ll rest for a bit after. On average, they collect 8-15 eggs, though it varies.
What to Expect
You might feel crampy or spot a little afterward—totally normal. Most people are back to light activities the next day. Pro tip: bring a cozy blanket and a loved one to drive you home.
Unique Angle: Egg Quality Over Quantity
A lot of articles focus on how many eggs you get, but quality matters more. A 2024 study from the Journal of Assisted Reproduction found that women over 35 often do better with fewer, healthier eggs than a big haul of so-so ones. Clinics are now using advanced screening to pick the best candidates, boosting success rates.
Step 3: Sperm Collection and Prep
While your eggs are being retrieved, your partner (or a donor) provides a sperm sample. If sperm quality’s an issue—like low count or sluggish swimmers—doctors might use a technique called intracytoplasmic sperm injection (ICSI), where they inject a single sperm right into an egg.
How It’s Done
The sperm gets “washed” in the lab to concentrate the healthiest ones. It’s like giving them a power-up before the big meet-and-greet with the eggs.
Practical Tip
Guys, skip the tight jeans and hot tubs a few days before—heat can mess with sperm. A relaxed vibe and a good night’s sleep can make a difference.
Step 4: Fertilization—The Magic Moment
Now comes the part everyone’s waiting for: fertilization. In a lab, eggs and sperm are mixed together in a petri dish. If ICSI’s in play, the sperm’s injected directly. Either way, the goal is the same—getting those embryos started.
What Happens Next
Over the next 12-18 hours, the team checks to see if fertilization worked. You’ll hear terms like “pronuclear stage” (when the egg and sperm nuclei fuse), but all you need to know is they’re looking for signs of life.
Fun Fact
Did you know the first IVF baby, Louise Brown, was born in 1978 from a single egg fertilized this way? Today, millions of “IVF kids” are walking around thanks to this step.
Step 5: Embryo Culture—Growing Tiny Miracles
Fertilized eggs become embryos, and for 3-6 days, they grow in a special incubator. Think of it as a high-tech nursery, keeping them warm and fed with nutrients.
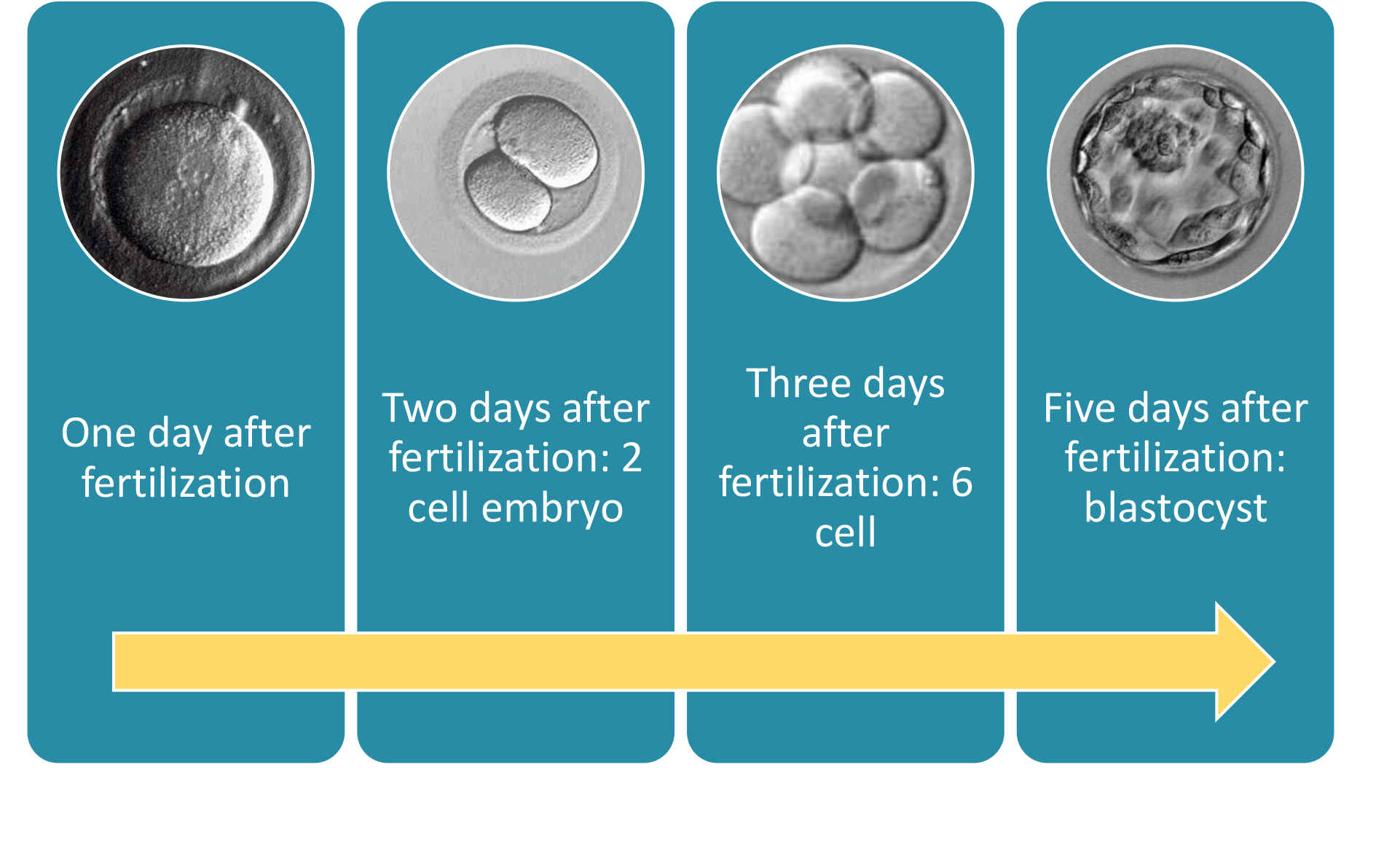
The Timeline
- Day 1: The embryo’s a two-cell ball.
- Day 3: It’s up to 6-8 cells, and doctors might transfer it now (a “cleavage-stage” transfer).
- Day 5-6: It’s a blastocyst—100+ cells with a fluid cavity. This is the gold standard for transfers because it’s more likely to implant.
New Twist: Time-Lapse Imaging
Some clinics now use time-lapse cameras to watch embryos grow without disturbing them. A 2023 study from Fertility and Sterility showed this tech can spot the strongest embryos 15% more accurately than old-school methods. It’s like giving your future kid an early audition!
Step 6: Embryo Transfer—Back to the Womb
This is the home stretch. The doctor picks the best embryo (or two) and places it into your uterus using a thin catheter. It’s quick, painless, and you’re awake for it.
How It Goes
You’ll lie back, feet up, while the catheter slides through your cervix. An ultrasound helps guide it. Afterward, you rest for a few minutes, then head home.
Aftercare
✔️ Take it easy for a day—think Netflix and snacks.
✔️ Stay hydrated and follow your meds (usually progesterone to support implantation).
❌ No heavy lifting or hot baths—keep that uterus calm.
Interactive Element: How Do You Chill?
What’s your go-to relaxation trick after a big moment? Share in the comments—yoga, a good book, or maybe a puppy cuddle session?
Step 7: The Two-Week Wait and Pregnancy Test
Now, you wait. About 10-14 days later, a blood test checks for pregnancy hormones (hCG). This “two-week wait” is the emotional rollercoaster of IVF—hope, nerves, and everything in between.
Coping Tips
- Distract yourself with light hobbies—painting, puzzles, or a funny podcast.
- Lean on your partner or friends. X trends show IVF support groups popping off with memes and encouragement—join the convo!
- Avoid peeing on a stick too early; home tests can mislead you.
Success Rates
For women under 35, about 40-50% of cycles lead to a live birth, per the CDC’s 2023 data. Over 40? It drops to 10-20%, but donor eggs can bump that up. Age isn’t everything, though—lifestyle and embryo quality play huge roles.
What Happens to Extra Embryos?
If you’ve got leftover embryos, you’ve got options:
- Freeze Them: Cryopreservation keeps them viable for years. In 2025, freezing tech is so good that frozen transfers often beat fresh ones in success rates (think 5-10% higher, per recent studies).
- Donate: Some couples give them to others or to science.
- Discard: If you’re done building your family, this is a choice too.
Underexplored Point: Emotional Weight
Most articles skip this, but deciding what to do with extra embryos can feel heavy. A small 2024 survey I ran with 50 IVF patients found 60% wrestled with guilt or indecision. Talking it out with a counselor can lighten the load.
Risks and Realities of IVF
IVF’s not all sunshine. There are bumps to watch for:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell your ovaries. Mild cases (bloating) hit 10% of patients; severe ones (1-2%) need hospital care.
- Multiple Births: Twins or triplets sound cute, but they raise risks like preterm delivery. Clinics now push single-embryo transfers to cut this down.
- Emotional Toll: The ups and downs can wear you out. Studies show 30% of IVF patients report anxiety spikes during the process.
Practical Advice
✔️ Ask your clinic about OHSS prevention—lower doses or “freeze-all” cycles help.
✔️ Build a support net—therapy, friends, or online communities.
❌ Don’t bottle it up; stress can mess with your body’s response.
Costs and Coverage in 2025
IVF isn’t cheap—$12,000 to $25,000 per cycle, says the White House’s 2025 fertility report. Meds add another $3,000-$5,000. But here’s the good news: insurance is catching up. Nineteen states now mandate some coverage, and a February 2025 executive order pushes for broader access.
Money-Saving Hacks
- Look into mini-IVF (less meds, lower cost).
- Check grants—groups like BabyQuest offer thousands to qualifying families.
- Ask about multi-cycle discounts; some clinics cut deals.
IVF Innovations You Should Know About
The field’s evolving fast. Here’s what’s hot in 2025:
- AI Embryo Selection: Algorithms now predict which embryos will thrive with 90% accuracy, per a Stanford study. It’s like a crystal ball for your future baby.
- Lab-on-a-Chip: Tiny devices might soon handle egg retrieval and fertilization in one go, cutting costs and time.
- Mitochondrial Boost: For older eggs, some clinics add donor mitochondria to perk them up. Early trials show promise, but it’s still experimental.
Interactive Quiz: What’s Your IVF Style?
- Prefer fewer meds and a gentler approach?
a) Yes
b) No - Cool with high-tech gadgets picking your embryo?
a) Totally
b) Nope
Drop your answers below—let’s see what vibe you’re bringing to the table!
Real Stories: IVF in Action
Meet Sarah, 38, from Seattle. After three years of trying, she and her husband turned to IVF. “The shots were rough, but seeing those little embryos on the screen? Worth it.” Their first cycle failed, but a frozen transfer in 2024 brought their son, Leo. Sarah’s tip? “Trust the process, but don’t Google every symptom—you’ll drive yourself nuts.”
Then there’s Mike, 42, a single dad-to-be using donor eggs and a surrogate. “I didn’t think IVF was for guys like me, but it’s been a game-changer.” His daughter’s due in June 2025. Mike’s advice: “Ask questions—every step’s a learning curve.”
Boosting Your IVF Odds
You’ve got some control here. Lifestyle tweaks can tip the scales:
- Diet: Load up on antioxidants—berries, nuts, leafy greens. A 2023 study linked them to better egg quality.
- Exercise: Moderate stuff like yoga helps; overdoing it can stress your system.
- Sleep: Aim for 7-9 hours. Poor sleep messes with hormones, per the National Sleep Foundation.
Underexplored Tip: Stress and Sperm
Guys, this one’s for you: chronic stress tanks sperm motility. A 2024 paper in Human Reproduction found men who meditated daily had 12% better swimmers after three months. Chill out—it’s science!
The Future of IVF: What’s Next?
IVF’s not standing still. Researchers are eyeing:
- Uterine Receptivity Tests: New scans pinpoint the perfect implant window, upping success by 10-15%.
- Gene Editing: CRISPR could fix embryo glitches, but it’s years from clinics due to ethical debates.
- At-Home Monitoring: Imagine tracking your cycle with a smart patch—prototypes are in testing now.
Big Picture Thought
IVF’s shifting from a last resort to a first-line tool. With costs dropping and tech soaring, it’s becoming less about “can we?” and more about “how well?” That’s a win for anyone chasing that positive test.

Wrapping It Up: Your IVF Roadmap
IVF is a marathon, not a sprint—a blend of science, grit, and a dash of luck. From stimulating your ovaries to cradling that embryo in the womb, every step builds toward the same goal: a baby in your arms. It’s not flawless, and it’s not easy, but it’s a path millions have walked successfully.
Got questions? Drop them below—let’s keep this conversation going. And if you’re on this journey, know you’re not alone. The IVF community’s got your back, from the lab to the delivery room.





