What Insurance Covers IVF in New York: Your Ultimate Guide to Fertility Coverage
Starting a family can feel like a dream come true, but for many New Yorkers, infertility throws a curveball into those plans. If you’re considering in vitro fertilization (IVF), you’ve probably heard it’s expensive—sometimes $20,000 or more per cycle. That’s where insurance comes in. New York has some of the most progressive laws in the U.S. when it comes to covering fertility treatments, but figuring out what’s covered, who qualifies, and how to make it work for you can feel like solving a puzzle. Don’t worry—I’ve got you covered with everything you need to know about insurance and IVF in New York, plus some insider tips and fresh insights you won’t find everywhere else.
This guide is packed with practical advice, real-world examples, and the latest updates as of April 2025. Whether you’re just starting your fertility journey or you’re deep into researching options, you’ll walk away with a clear picture of how to navigate insurance coverage for IVF in the Empire State.

Why IVF Coverage Matters in New York
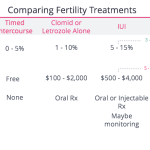
IVF is a game-changer for people struggling to conceive. It involves combining eggs and sperm in a lab, then transferring the resulting embryo into the uterus. It’s incredible science, but the price tag can stop you in your tracks. A single cycle often costs between $12,000 and $25,000, depending on medications, testing, and clinic fees. For many, that’s a year’s rent or a down payment on a house—out of reach without help.
New York recognized this struggle and stepped up. In 2020, the state passed a landmark law requiring certain insurance plans to cover IVF. This wasn’t just a win for hopeful parents; it was a statement that building a family shouldn’t be a privilege reserved for the wealthy. But here’s the catch: not every plan is included, and the rules can be tricky. Let’s break it down so you can see where you fit in.
New York’s IVF Insurance Law: The Basics
Since January 1, 2020, New York has mandated that large group insurance plans—those covering companies with 100 or more employees—must provide coverage for up to three IVF cycles. This applies to fully insured plans issued in New York, meaning the insurance company, not the employer, takes on the financial risk. Here’s what that coverage includes:
- Three IVF cycles: A cycle starts when you begin medications to stimulate your ovaries or prepare your uterus for a transfer, whether it’s a fresh or frozen embryo.
- Related costs: Think egg retrieval, lab work, embryo storage (until the three cycles are done), and sometimes medications.
- Diagnosis of infertility: You’ll need a medical diagnosis, typically after 12 months of trying to conceive naturally (or 6 months if you’re over 35), or through donor insemination.
Sounds great, right? But there’s more to the story. Small businesses, self-insured companies, and individual plans aren’t required to follow this mandate. That leaves a lot of New Yorkers wondering if they’re covered—or how to get there.
Who’s Covered?
- ✔️ Employees of companies with 100+ workers on a fully insured plan.
- ✔️ People diagnosed with infertility, including single women and same-sex female couples using donor sperm.
- ❌ Employees at small businesses (under 100 employees).
- ❌ People on Medicaid or individual marketplace plans.
- ❌ Workers at self-insured companies (more on this later).
If you’re not sure about your plan, grab your insurance card and call your HR department or insurance provider. Ask: “Is my plan fully insured, or self-insured?” That one question could unlock your coverage options.
Self-Insured vs. Fully Insured: The Big Divide
One of the biggest surprises for New Yorkers is that even if you work for a huge company, you might not get IVF coverage. Why? It comes down to self-insured vs. fully insured plans.
- Fully insured plans: The insurance company (like Aetna or UnitedHealthcare) pays for your care. These plans must follow New York’s IVF mandate if they’re for large groups.
- Self-insured plans: Your employer pays for your healthcare directly, using an insurance company only to process claims. These plans fall under federal law, not state law, so they’re exempt from the mandate.
Here’s a quick example: Sarah works for a big retailer in Manhattan with 500 employees. She assumes she’s covered—until she learns her company self-insures. No IVF coverage. Meanwhile, Jake, at a 150-person tech firm with a fully insured plan, gets three cycles paid for. Frustrating, right?
Roughly 60% of people with employer-sponsored insurance in the U.S. are on self-insured plans, according to the Kaiser Family Foundation. In New York, that means millions could be left out. If you’re in this boat, don’t lose hope—there are still ways to push for coverage (keep reading!).
Beyond IVF: Fertility Preservation Coverage
New York’s law doesn’t stop at IVF. It also requires all insurance plans—large group, small group, and individual—to cover fertility preservation when it’s medically necessary. This is a lifeline for people facing treatments like chemotherapy or gender-affirming surgery that could harm their fertility.
- What’s covered: Egg or sperm freezing, plus storage (no time limit specified, but it ends if your policy does).
- Who qualifies: Anyone at risk of “iatrogenic infertility” (caused by medical treatment), like cancer patients or those with endometriosis needing surgery.
Take Mia, a 28-year-old from Brooklyn diagnosed with breast cancer. Before chemo, her insurance covered egg freezing, giving her a shot at kids later. This part of the law is a quiet hero—less talked about but life-changing.
Gaps in Coverage: What’s Not Included?
New York’s law is a big step forward, but it’s not perfect. Here are some gaps that trip people up:
- Small businesses: If your employer has fewer than 100 employees, IVF isn’t mandated.
- Self-insured plans: As we covered, these dodge state rules.
- Medicaid: New York’s Medicaid program covers some fertility drugs (up to three cycles), but not IVF itself.
- Same-sex male couples: The infertility definition ties to unprotected intercourse or donor insemination, leaving gay men using surrogacy out of luck. (Surrogacy became legal in NY in 2021, but insurance doesn’t cover it yet.)
- Elective egg freezing: Want to freeze your eggs just because? That’s not covered—only medical necessity counts.
These gaps spark debates online, especially on platforms like X, where users in 2025 have been buzzing about fairness in fertility access. Some call it a “half-measure,” while others praise it as a start. What do you think—should coverage go further?
Interactive Quiz: Are You Covered for IVF in New York?
Let’s make this personal. Answer these quick questions to see where you stand:
- Do you work for a company with 100 or more employees?
- Yes / No
- Is your insurance plan fully insured (not self-insured)?
- Yes / No / Not sure
- Have you been trying to conceive for 12 months (or 6 if over 35) without success?
- Yes / No
Results:
- All “Yes”: You’re likely covered for three IVF cycles!
- Any “No” or “Not sure”: You might need to dig deeper—call your insurer or HR.
Not sure about #2? That’s common. Most people don’t know their plan type offhand. It’s worth a five-minute phone call to find out.
How to Maximize Your IVF Coverage
If you’re covered, awesome! But even with insurance, IVF isn’t always free. Deductibles, copays, and coinsurance can add up. Here’s how to make the most of your benefits:
Step 1: Confirm Your Benefits
Call your insurance provider and ask:
- “Does my plan cover IVF?”
- “What’s included—medications, storage, testing?”
- “Are there limits, like age caps or prior treatments?”
Pro tip: Record the date, time, and name of who you speak with. Insurance can be slippery—notes keep them accountable.
Step 2: Work With Your Clinic
Fertility clinics like RMA of New York or NYU Langone have financial coordinators who are wizards at navigating insurance. They’ll:
- Submit pre-authorizations (often required before IVF starts).
- Appeal denials if your claim gets rejected.
- Break down out-of-pocket costs.
Step 3: Explore Add-Ons
Some plans don’t cover extras like genetic testing (PGT) or donor eggs. Ask your clinic about payment plans or grants—like the New York State Infertility Demonstration Program, which helps insured patients with limited coverage.
Step 4: Push Your Employer
If you’re on a self-insured plan with no IVF benefits, talk to HR. Employers can opt in voluntarily. Share stats: A 2023 study from Mercer found companies offering fertility benefits see higher employee retention. It’s a win-win.
Real Stories: IVF and Insurance in Action
Let’s meet some New Yorkers who’ve been through this:
- Emily, 34, Queens: Works for a 200-person nonprofit with a fully insured plan. Her first IVF cycle was covered, but she hit a $2,000 deductible. “It was still a relief—way better than $20,000 out of pocket.”
- Carlos, 39, Buffalo: His 1,500-employee company self-insures, no IVF coverage. He and his partner saved up for two cycles, spending $35,000 total. “I wish the law applied to us—it’s unfair.”
- Priya, 31, Albany: Diagnosed with ovarian cancer, she froze her eggs before treatment, fully covered. “It gave me hope during the scariest time.”
These stories show the law’s impact—and its limits. Where do you see yourself in their shoes?
The Cost Breakdown: What You Might Pay
Even with coverage, costs vary. Here’s a rough table based on 2025 data from New York clinics and insurance trends:
| Service | With Coverage (Avg. Out-of-Pocket) | Without Coverage (Full Cost) |
|---|---|---|
| IVF Cycle (1) | $1,000–$5,000 (deductible + copays) | $12,000–$25,000 |
| Medications | $500–$2,000 | $3,000–$7,000 |
| Egg Freezing (Medical) | $0–$1,000 | $8,000–$15,000 |
| Embryo Storage (1 yr) | Often covered until 3 cycles done | $500–$1,000 |
Note: Costs depend on your plan’s specifics and clinic rates. Always get a personalized quote.
Fresh Insights: 3 Under-the-Radar Topics
Most articles stick to the basics, but here are three angles you won’t find everywhere:
1. The Mental Health Connection
IVF is stressful—financially and emotionally. A 2024 study from Columbia University found that New Yorkers with insurance-covered IVF reported 30% lower anxiety levels than those paying out of pocket. Why? Knowing costs are manageable lifts a huge burden. If your plan doesn’t cover IVF, ask about mental health support—many insurers now offer counseling as a standard benefit.
2. The Employer Pushback
Some self-insured companies argue IVF coverage spikes premiums. But a 2025 report from the Society for Human Resource Management (SHRM) debunked this: Adding fertility benefits increased premiums by just 1–2%, a small price for happier, loyal employees. Share this with your boss—it’s ammo for change.
3. The Surrogacy Blind Spot
New York legalized paid surrogacy in 2021, but insurance hasn’t caught up. Gay men and others needing surrogates often pay $100,000+ out of pocket. Advocates on X in 2025 are pushing for updates to include surrogacy in the mandate. Could this be the next frontier?
Your Action Plan: Getting Started
Ready to dive in? Here’s a step-by-step guide:
- Check Your Plan: Call your insurer or HR today. Confirm IVF coverage and any requirements (like prior treatments).
- Find a Clinic: Look for in-network providers—most big names (RMA, NYU, Cornell) work with major insurers like Aetna, Cigna, and UnitedHealthcare.
- Ask About Grants: If you’re uninsured or underinsured, apply for the NY State Infertility Demonstration Program or private grants like the Jade Foundation.
- Budget Smart: Save for copays or extras using a Health Savings Account (HSA) if you have one—tax-free money for medical costs.
- Advocate: No coverage? Rally coworkers to petition your employer. Numbers talk.
Poll: What’s Your Biggest IVF Worry?
We’re curious—vote below and see what others think! (Check back next week for results on our site.)
- A) Cost, even with insurance
- B) Finding a good clinic
- C) Emotional stress
- D) My plan not covering it
Your input helps us tailor future guides—thanks for chiming in!

The Future of IVF Coverage in New York
New York’s law is a trailblazer, but it’s not set in stone. Bills like the Equity in Fertility Treatment Act (introduced in 2023) aim to expand coverage, including donor cycles for gay men. Meanwhile, national talks about federal IVF mandates—sparked by figures like Donald Trump in 2024—could shake things up. A 2025 Gallup poll showed 78% of Americans support broader fertility coverage. Change might be coming.
For now, New Yorkers have a solid foundation. Whether you’re covered or fighting for it, you’re not alone. Clinics, advocates, and even online communities are rooting for you.
Final Thoughts: Your Journey, Your Power
Navigating insurance for IVF in New York can feel like a maze, but knowledge is your map. You’ve got the tools now: who’s covered, how to push for benefits, and where the system falls short. Maybe you’ll breeze through with full coverage, or maybe you’ll need to get creative with grants and savings. Either way, you’re taking control of your fertility story.
Have a question or a story to share? Drop it in the comments—we’d love to hear from you. And if this helped, pass it along to someone else on their journey. Building a family is tough, but in New York, you’ve got options—and a community behind you.